Today, 82% of adults in the U.S. regularly take at least one medication, while 29% take five or more. Unfortunately, many aren’t taking them as prescribed.1
Medication adherence has been a significant challenge in the U.S. for years and continues to drive up health care costs and lead to poor clinical outcomes for patients. The financial and health implications are staggering: poor medication adherence takes the lives of 125,000 people a year and costs the U.S. healthcare system nearly $300 Billion.2
Non-adherence includes not filling a prescription or delaying a refill, skipping doses, or stopping a medication on one’s own. Adherence is especially important in chronic conditions, where symptoms are persistent and require ongoing medical attention. For most chronic conditions adherence rates of at least 80% are needed for a medication to be most effective, but it is estimated that about half of Americans do not take medications regularly as prescribed.3
ADDRESSING BARRIERS TO ADHERENCE
So why are people not taking their medications as prescribed? Understanding the barriers affecting your members is a critical step in developing programs that drive results.
A member may not take his or her medication properly for many reasons. The graphic below depicts the top barriers to medication adherence including time management, limited knowledge, physician-related issues, lack of motivation, side effects, physical limitations, financial and other barriers. These are unique for each member and some members may struggle with multiple. 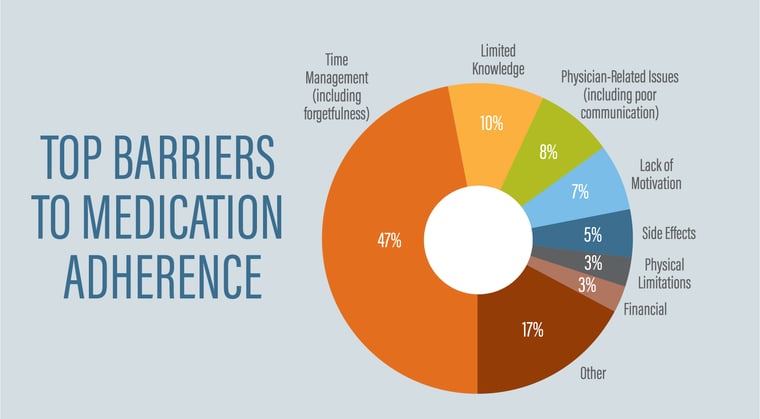 Source: Health Dialog. The Roadmap to Medication Adherence: 6 Critical Steps That Drive Success.
Source: Health Dialog. The Roadmap to Medication Adherence: 6 Critical Steps That Drive Success.
By addressing adherence, you can help members tackle these barriers and improve care. When members take their medications as prescribed, they have better health outcomes and are less likely to experience complications that can increase medical costs in the future, such as doctor visits and hospitalizations. Indirect costs, such as missed work days due to medical conditions, can also decrease with better adherence. Adherence can also help improve members’ condition management and quality of life.
MEASURING ADHERENCE
Many different methods measure medication adherence. One common method is self-reports from members themselves, which can be a single screening question such as “In the past month, how many doses of your medication have you missed?” While this method is quick and simple, it is often an optimistic estimate of adherence influenced by inaccurate recall.
Another common method to measure adherence is using electronic pharmacy claims data. By looking at when a member refills their medication, we can determine how much medication a patient has on hand over a period of time and can identify gaps in therapy. This method is objective and can provide a more accurate estimate of a member’s medication adherence, although no one method is perfect.
INTRODUCING AN EFFECTIVE SOLUTION
Many organizations are implementing programs that reduce costs and create positive patient outcomes, one being Pharmacoadherence. A Pharmacoadherence program identifies non-adherent members taking their medication as prescribed less than 80% of the time, according to pharmacy claims data. Intervention letters are sent to the member and/or the prescriber, depending on the specific program.
The program can be run for any chronic condition. Some examples include cholesterol, diabetes, hypertension, depression, rheumatoid arthritis, and ADHD.
The goal of the Pharmacoadherence program is to help coordinate care between the member and prescriber and improve the member’s education about their chronic condition and medication. Outcomes are reported at 6 and 12 months after the intervention to measure improved adherence.
DELIVERING RESULTS
Navitus’ Pharmacoadherence program has shown positive outcomes in previous years and is proving to be valuable in improving member health. Below are some of our 2019 program highlights:
-03.png?width=760&name=the-roadmap-to-medication-adherence%20(1)-03.png)
Ask your PBM or your Navitus account representative if an adherence program is available, and if so, how it can benefit you and your members.
Interested in finding additional ways to reduce expenses and improve member health? Download our e-book, 3 ways to improve your Rx benefit plan performance.

1. Centers for Disease Control and Prevention
2. National Center for Journal of Medicine
3. Kim J, Combs K, Downs J, Tilman F. Medication adherence: the elephant in the room.
US Pharm. 2018;43(1):30-34.





