It’s no secret that growing prescription drug costs are causing concern for plan sponsors and their members.
Pharmacy benefits can be complicated, but the solution to effectively balance costs and value doesn’t have to be. You can effectively combat wasteful spend in your pharmacy benefits plan by taking a closer look at your drug mix and formulary approach.

IDENTIFYING WASTEFUL OR LOW-VALUE DRUGS
Plan sponsors continually search for the “recipe for success” to formulary management. It starts by finding the right product mix. You need to determine which drugs deliver the most value and which ones you should “boot” off your list. Formularies can often include drugs that have little to no clinical value and drive up costs, often referred to as wasteful or low-value drugs.
Examples of wasteful or low-value drugs include:1
- ‘Me-Too Drugs,’ which are very similar to an existing drug, but with a minor ingredient change, creating a new drug that doesn’t add any clinical value.
- Combination drugs, which combine two or more active ingredients into one, and can often increase the cost above and beyond what the ingredients would cost individually.
- Prescription drugs that are presented to patients when other clinically-effective over-the-counter (OTC) alternatives are available, often at a lower cost.
- Brand-name drugs that are offered when lower-cost, equivalent generics are available.
The table below demonstrates how wasteful and low-value drugs affect formulary management and negatively impact plan sponsors.
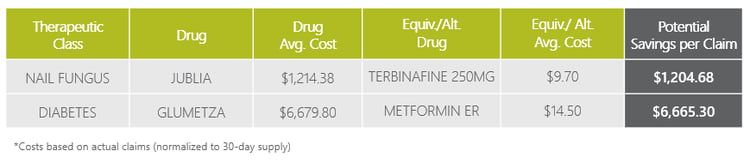
Let’s take Jublia® for example, it is a fairly expensive brand medication that does not offer any clinical advantage over Terbinafine. As you can see from the table above, the average cost of Jublia is around $1,200 for a 30-day supply. With a recommended treatment duration of 48 weeks, that comes to over $14,000! In comparison, Terbinafine is a clinically-effective alternative drug that costs less than $10 for a 30-day supply. With a recommended treatment duration of 12 weeks, that’s a total of only $30.
Another example is Glumetza®, an extended release version of Metformin, which is a first-line treatment for diabetes. Metformin has been on the market for a long time and it is very inexpensive, less than $15 for a 30-day supply. In comparison, Glumetza costs over $6,600 for a 30-day supply!
According to a recent study that evaluated the impact of excluding wasteful drugs across a group of plan sponsors, wasteful prescriptions represented up to 12% of total claims.1 The study results revealed that ten drug groups accounted for 72% of total savings and eight drugs, removed from the formularies, accounted for 21% of the total savings.1
TACKLING FORMULARY MANAGEMENT
Managing your formulary is critical to your plan’s performance. Unnecessary costs can multiply if left unchecked, so it’s important to consider what approach to formulary management your plan is using.
A rebate-focused approach focuses on attaining higher rebates, which can lead to selecting higher-cost drugs. Big rebates may appear to generate more savings, but it’s important to pay attention to the drug cost. You may be spending more to get more rebates, but your overall costs may actually be higher.
Traditional PBMs will often use a rebate-focused approach to generate spread (also known as margin or mark-up) on rebates. With the goal of achieving higher rebates, these PBMs will select the most profitable drugs for formulary placement to increase spread.
Employers and other organizations may be starting to realize there’s an issue. According to a recent study, 75% of employers do not believe rebates are an effective tool to help drive down pharmaceutical costs.2 In addition, 90% said they would welcome an alternative to a rebate-driven approach to formulary management.2
Instead, a lowest-net-cost strategy focuses on recommending lower-cost alternatives, such as generics or less expensive brands, based on clinical guidelines. It uses rebates and a lower average wholesale price (AWP) starting point to lower all-in per member per month (PMPM) costs.
The pass-through PBM model fully supports a lowest-net-cost approach by making sure 100% of all rebate revenue is passed directly back to the plan sponsor. Since its only revenue source is an admin fee and no spread is involved, the pass-through model ensures the PBM does not have misaligned incentives to prioritize higher-cost drugs for formulary placement to increase spread.
A lowest-net-cost approach can cost 10% less than a rebate-focused formulary.3
ACHIEVING A HIGH-VALUE DRUG MIX AND REDUCING SPEND
The good news is, it is possible to establish a high-performance formulary that provides members with access to quality, clinically-effective medications that improve health and deliver the lowest net cost.
Transparency is the key to exposing wasteful drugs. Look beyond rebates, and instead focus on clinically-effective, lowest-net-cost drugs. Identify and remove wasteful drugs from your formulary, and make sure your formulary works for you and aligns with your goals. Start by monitoring utilization and developing a transition plan that will minimize member impact.
Take a look at your formulary – not just for the specific drugs in the example above, but for any drugs that are wasteful or low-value. At the very least, make sure these drugs have prior authorization (PA) criteria in place.
Ask your PBM or consultant:
- Are any members utilizing these products?
- What is the PA criteria for approval?
- What is the net cost of the drug after rebates?
If you can’t get the answers to those questions, you should consider – why not? If your formulary contains wasteful or low-value drugs, you are spending more than you should.
By staying actively involved in your formulary management decisions, you will significantly reduce the impact of prescription drug price increases on your plan and your members.
Want to learn more strategies to help you optimize your formulary? Download our e-book today!

- Vela, L. Reducing Wasteful Spending in Employers’ Pharmacy Benefit Plans. https://www.commonwealthfund.org/publications/issue-briefs/2019/aug/reducing-wasteful-spending-employers-pharmacy-benefit-plans. Published August 30, 2019. Accessed January 3, 2020.
- Combs, B. How Employers are Shaking Up Pharmacy Benefits for 2019. www.cnbc.com/2018/08/07/how-employers-are-shaking-up-pharmacy-benefits-for-2019.html Published August 7, 2018. Accessed January 3, 2020.
- Navitus internal data analysis, 2019.





