Utilization management (UM) programs serve as a gatekeeper to the formulary, working to ensure appropriate, cost-effective medication use. They can be great tools to help plan sponsors fine tune plan performance and lower drug costs, if used effectively.
In fact, using UM programs to transition high-cost brand prescriptions to low-cost generic options can reduce drug spend by up to 30%.1
An effective UM strategy strikes a balance between managing pharmacy benefit costs and ensuring members have access to the most clinically appropriate, safe and cost-effective medications. For plan sponsors, it’s also important to consider how well your PBM’s UM strategies align with your goals.
EXPLORING UM PROGRAMS
Examples of UM programs include step therapy, quantity limits and prior authorization.
- Step therapy (ST) promotes clinically effective, lower-cost medications before starting or “stepping-up” to a higher-cost therapy.
- Quantity limits (QL) limit medication dispensing by time frame and/or dosage.
- Prior authorization (PA) requires the prescriber to obtain approval from the insurer prior to dispensing a prescribed medication.
IMPLEMENTING EFFECTIVE UM STRATEGIES
One of the most frequently used UM tools is PA. PA can be a beneficial tool to ensuring the prescribed medication is appropriate according to evidence-based clinical guidelines and is the most cost effective. The problem is, no industry standard for PA criteria exists. Plus, PA acceptance rates can vary significantly across PBMs. Depending on your PBM’s approach it may not be saving you as much as it could.
In a traditional model, PBMs generate revenue from rebates and pharmacy transactions, called spread. Traditional PBMs that have a rebate-focused formulary are incentivized to approve as many claims as possible to increase spread revenue. In comparison, a pass-through PBM's only source of revenue is an admin fee, instead of generating income from rebates and pharmacy transactions. Pass-through PBMs that have a lowest-net-cost formulary strategy don’t take spread, so they do not benefit from a higher claim approval rate, and instead will focus on recommending lower-cost alternatives that are based on clinical guidelines.
A lowest-net-cost approach paired with the right UM programs can cost 10% less than a rebate-focused formulary.1
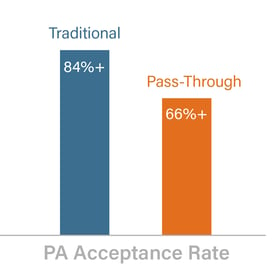 In a recent study that evaluated PBMs’ prior authorization approval ratings, traditional PBMs had an average PA approval rate of 84% or more, while pass-through PBMs had an average approval rate of 66% or less.2 The study revealed that, in general, high PA approval rates may lead to higher overall drug spend.
In a recent study that evaluated PBMs’ prior authorization approval ratings, traditional PBMs had an average PA approval rate of 84% or more, while pass-through PBMs had an average approval rate of 66% or less.2 The study revealed that, in general, high PA approval rates may lead to higher overall drug spend.
EVALUATING COSTS AND ACHIEVING SAVINGS
While UM programs are intended to help plans to better manage drug spend, it’s important to consider any additional fees that might be associated with using UM programs. For example, some PBMs charge a per-review fee, which could range from $25 to $60 per review.2 Others may charge a per-claim fee or per member per month (PMPM) pricing fee for bundled UM program packages, or PMPM fees for a-la-carte programs.2
Manufacturers may offer higher rebates for loose PA criteria, but spending more to get more rebates doesn’t justify using the “approve more” approach. Appropriate UM criteria can help identify opportunities to move expensive brands to lower-cost options, resulting in significant savings. Foregoing rebates for tighter PA criteria often results in a lower net cost since the focus is to promote the appropriate utilization of lower-cost alternatives first.
There is no “one size fits all” solution to implementing effective UM strategies. Plan sponsors should evaluate their population needs and plan goals and consider how to apply UM programs to work smarter when it comes to determining appropriate, cost-effective drug use and reducing costs.
Want to learn more strategies to improve your Rx benefit plan performance? Download our e-book today!

- Navitus Internal Data Analysis, 2019.
- Managing the High and Rising Cost of Prescription Drug Coverage. Segal Consulting. https://www.segalco.com/publications-videos/data/#Multiemployer. Published Fall 2017.





