If you answered yes, then you’re not alone. In the wake of COVID-19 many plan sponsors are looking for additional ways to save on their pharmacy benefit plan. How can you do that?
Have you ever considered a narrow pharmacy network strategy? Find out why it might be time to start.
In today’s blog, we’ll explore a few key aspects of pharmacy network management and answer the most common questions plan sponsors have when it comes to implementing network changes.

Plan sponsors should consider several factors when evaluating a network management strategy, including cost management, pharmacy accessibility and member disruption. One thing to keep in mind is the savings opportunity. With narrow networks your PBM makes agreements with certain pharmacies for better rates, which can mean greater savings for you.
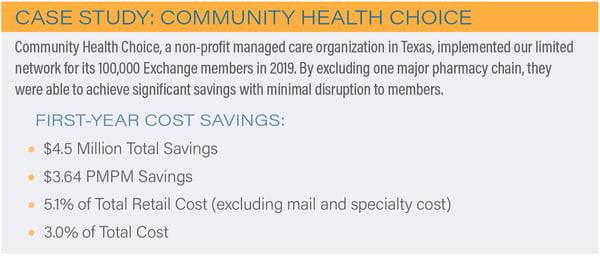
In 2019, Navitus’ narrow network saved plan sponsors an average of 3-5% on their annual retail drug spend, with some saving as much as 10%. Seeing the value of these savings, 25% more clients adopted this network in 2019 over the previous year.1
So, how do plan sponsors know if a narrow network strategy is right for them or not? Here’s what you need to know:
What is the Benefit of a Narrow Network Management Strategy?
A narrow network management strategy can serve as an effective alternative to the traditional broad or open pharmacy network to help lower drug spend and improve plan performance. Narrow networks are designed to provide deeper minimum network discount performance, encourage members to use certain pharmacies through benefit design and optimize member convenience and access.
- A preferred network provides deeper discounts at preferred pharmacy chains. Members are not restricted from using the broad network pharmacies, but are incentivized with a lower copay to use preferred pharmacies.
- A limited network is a deeply discounted network that limits pharmacy participation through contractual design, while continuing to offer excellent access. This network excludes one or more pharmacy chains and provides plans with the flexibility to accommodate unique needs, while better controlling costs.
How do Pharmacy Network Offerings Differ Across PBMs?
While all pharmacy benefit managers (PBMs) offer network management, the strategy across PBM models can vary greatly. Traditional PBMs take spread on retail pharmacy costs, and many even have an ownership interest in retail pharmacies, which can incentivize those PBMs to align network strategies with their own interests.
In comparison, a pass-through PBM immediately passes on all network reimbursement improvements, including all upside performance, to the plan sponsor for the contract’s full life. Narrowing the network can come through various means, including:
-
Outright exclusion of higher cost pharmacies
-
Differential copays between preferred and non-preferred pharmacies
-
90-day at retail limited to a select group of pharmacies for acute and maintenance medications
The bottom line - an effective narrow network strategy should focus on offering plans the biggest financial advantage while meeting member needs, rather than increasing revenue for the PBM.
ARE Narrow Network Savings Really Worth the Member Disruption?
This is a very common question, especially in today’s current economic environment. Plan sponsors are looking for ways to lower costs, but increasing concerns about member disruption can often deter plans from exploring narrow network options. However, it is possible to implement a narrow network that generates savings for the plan, while maintaining a wide selection of pharmacies to promote member choice and convenience, and limit disruption.
When evaluating a pharmacy network strategy, PBMs can perform a comprehensive analysis to determine which pharmacies have high utilization and work those into the network design. Many big retail pharmacy chains tend to be within a five-mile radius of each other. Even if you exclude one large chain from the network, members will generally have access to another pharmacy nearby, which limits the impact and “noise” that many plan sponsors are concerned about.
According to a recent report, nearly 9 out of 10 Americans live within one mile of a community retail pharmacy. Even consumers who live in more rural areas are still typically within 6.3 miles of a pharmacy.2
But member disruption isn’t just about pharmacy location, it’s also about maintaining affordable prescription costs. In fact, members are often willing to switch pharmacies if it will reduce their out-of-pocket expenses. In a recent survey, 30% of Medicare Part D beneficiaries listed copay costs as the most important factor in their pharmacy selection, followed by pharmacy location at 18%.3
The key is to highlight the advantages that narrow networks bring to members.
Here are a few tips to effectively switch to a narrow network and minimize member disruption:
- Make the transition as easy as possible. For example, transition medications for members for the first 90 days to help ease the change and allow adequate time to begin using in-network pharmacies.
- Deploy proactive member communications well in advance of any pharmacy network changes. An effective member outreach strategy should highlight the benefits of a narrow network using a variety of communication methods including: print, intranet articles, newsletters and video.
- Implement major network changes over time to give members time to adjust to the new network.
Well-managed pharmacy networks are key to reducing plan sponsor costs without reducing member access. Choose what makes the most sense for your plan and members. Explore network options that offer the flexibility desired to meet plan goals, achieve cost savings and provide appropriate pharmacy access for members.
To learn more, check out our e-book, 3 Ways to Improve Your Rx Benefit Plan Performance.

- Navitus 2019 Drug Trend Report.
- The 2020 Economic Report on U.S. Pharmacies and Pharmacy Benefit Managers. Drug Channels Institute. Published March 2020. Accessed June 16, 2020.
- Prescription Drug Costs Are a Top Concern for Many Medicare Beneficiaries, Yet 34 Percent Aren’t Reviewing Part D Plans Before Renewal, Walgreens Survey Shows. Walgreens. https://news.walgreens.com/press-releases/general-news/prescription-drug-costs-are-a-top-concern-for-many-medicare-beneficiaries-yet-34-percent-arent-reviewing-part-d-plans-before-renewal-walgreens-survey-shows.htm. Published October 31, 2016. Accessed June 17, 2020.





