Find out how it works and why more plan sponsors are implementing solutions.
Electronic health (eHealth) programs are an essential part of a patient-centered health care experience, reducing administrative burden and improving care through access to real-time benefit information.
- 86% believe that it’s either extremely or very important to have patient-specific cost and coverage information at the point of prescribing1
- 97% believe it’s important to have cost-effective medication alternatives at the point of prescribing1
- 78% believe prior authorization (PA) delays cause treatment abandonment2
That’s where eHealth can play a crucial role.
WHAT IS eHealth?
eHealth is the combined use of electronic information and communication technology in the health care system.3 eHealth solutions streamline processes, minimize barriers along the prescription journey and provide a viable opportunity to optimize patient care through exchanging treatment-related data between patients and health care providers.3 It can also provide significant savings opportunities for plan sponsors and their members that might not otherwise have been visible.
Studies have shown cost and reimbursement uncertainty are key barriers in the health care system, often creating confusion and inefficiencies.4 A recent survey reported 67% of patients who went to pick up a prescription at the pharmacy found out it cost more than expected. As a result, over one-third left without their medication.5 eHealth solutions address barriers to health by promoting better cost and choice transparency and improving health care delivery.
Why eHealth mATTERS TO pLAN sPONSORS
eHealth solutions are shown to improve member health outcomes, reduce costs and increase overall plan and member satisfaction by:- Reducing turnaround times for prescribing decisions and PA processes
- Disseminating real-time benefit information at the point of care
- Improving formulary visibility and compliance
- Encouraging utilization of cost-effective alternatives at the point of prescribing
- Helping members get their medications more timely
- Identifying medication adherence issues
- Lowering overall drug spend
How it Works
Our eHealth solution includes a suite of programs that work in harmony to:
- Empower prescribers and members by giving detailed insight into the member’s benefits at the point of care
- Lower drug spend by providing timely medication alternatives
- Reduce administrative costs by increasing efficiencies
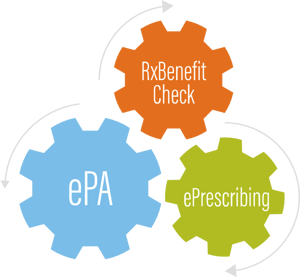 Electronic Prescribing (ePrescribing)
Electronic Prescribing (ePrescribing)
ePrescribing enables prescribers to electronically access patient medication history, prescription benefit and eligibility information. It provides prescribers insight into formulary status at the point of care and can serve as a gateway to other eHealth solutions.
In a recent study, when providers used eHealth solutions, such as ePrescribing, first and future fill adherence increased by 14-21%.6
Electronic Prior Authorization (ePA)
ePA is the automated process of exchanging member health and medication information that is required to determine drug plan coverage. Providers can submit a PA electronically at the time of prescribing, which affords an opportunity for prompt prescription changes if PA criteria are not met. ePA also helps avoid member trips to the pharmacy before their prescription is ready, and allows for a patient-prescriber discussion at the point of care, thereby reducing turnaround time.
A recent case study found that patients received their medications an average of 13.2 days sooner when providers submitted ePA requests at the point of prescribing, compared to requests started at the pharmacy.5
RxBenefit Check (RxBC)
RxBC, also known as real-time benefit check or real-time prescription benefit, is an inquiry or adjudication tool that provides up-to-the-minute benefit information to a provider through electronic health records (EHRs). RxBC gives the prescriber the ultimate insight into prescription benefits, including member cost at the pharmacy, formulary alternatives, lower-cost pharmacy channels and utilization management (UM) criteria.
Start embracing eHealth solutions as an essential part of the prescription process and experience the benefits of improved adherence, enhanced satisfaction and lower costs. Contact your account team today to learn more!
- Surescripts/GLG Script Writing Technology Evaluation Survey. Published 2016. Accessed April 8, 2021.
- 2017 AMA Prior Authorization Physician Survey. American Medical Association. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/arc/prior-auth-2017.pdf. Published February 2018. Accessed April 8, 2021.
- Tebeje TH, Klein J. Applications of e-Health to Support Person-Centered Health Care at the Time of COVID-19 Pandemic. Telemedicine and e-Health. https://www.liebertpub.com/doi/pdf/10.1089/tmj.2020.0201. Published July 31, 2020. Accessed December 10, 2020.
- Riggs KR, Ubel PA. Overcoming Barriers to Discussing Out-of-Pocket Costs With Patients. JAMA Intern Med. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4467553/. Published June 2014. Accessed April 8, 2021.
- 2021 Medication Access Report. CoverMyMeds. https://insights.covermymeds.com/medication-access-report?utm_medium=external&utm_source=guest-post&utm_campaign=mar-21&utm_term=drugchannels&utm_content=sponsored-link. Published January 29, 2021. Accessed March 22, 2021.
- Smith JY, Leslie RS, Patel BV, Kucharski C, Joseph SB, Sow M. E-Prescribing With Decision Support is Associated With Improvements in Medication Adherence. The American Journal of Pharmacy Benefits. https://www.pharmacytimes.com/view/eprescribing-with-decision-support-is-associated-with-improvements-in-medication-adherence. Published August 17, 2016. Accessed April 30, 2021.





