Navitus’ Senior Director of Population Health, Julie Olson, shares her unique perspective on how to work with your PBM to improve medication adherence and achieve lower plan costs.
Taking medications as directed is a critical component for improving health outcomes and preventing unnecessary medical costs. In fact, low medication adherence—when a patient’s behavior fails to correspond with their prescribed regimen, including time, dosage, duration and frequency of medication intake—negatively impacts the health of millions of Americans and costs the U.S. healthcare system up to $300 billion annually.
In addition to the unsustainable systemic implications associated with non-adherence, the problem also causes significant ramifications for plan sponsors, who consequently experience higher medical costs, lost earnings and lower productivity. What’s more, the pandemic has created lasting effects on our economy and healthcare system, prompting plan sponsors to take a closer look at how they support their members through their pharmacy benefits and promote the value of adherence.
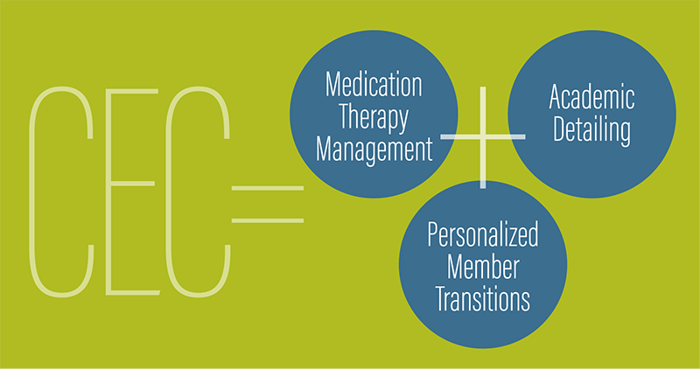
However, examining the best solution for members can be complex and require careful consideration of the various factors that may influence a member’s ability to adhere to their prescription regimen—including recent drug price hikes, lower-cost medication alternatives and potential gaps in care during benefits transitions. Leveraging pharmacy benefit management (PBM) tools designed to help members navigate critical crossroads on their prescription journey can help improve health outcomes and generate significant savings for both plan sponsors and members. At Navitus, we recently launched a new Clinical Engagement Center specifically designed to improve adherence and reduce costs through a three-pronged approach, consisting of Medication Therapy Management, Academic Detailing and Personalized Member Transitions. Here are a few considerations for how these interventions can help plan sponsors promote medication adherence among their members:
medication therapy management
Medication Therapy Management programs (MTMs) give plan sponsors the extra chronic condition support needed to improve members’ medication adherence. MTMs improve member/prescriber communications, offer customizable, CMS-compliant programs and deliver enhanced member support through medical review, consultations and outreach. This intervention model also reduces unnecessary expenses.
Through MTMs, members receive a Comprehensive Medication Review (CMR) with a pharmacist to review their medication regimen and develop an individualized action plan to ensure they get the most benefit from their medications. CMRs minimize the risk that a member fails to take his/her medications due to confusion or low health literacy by providing an opportunity for personalized clinical consults to help members better understand why and how they should take their prescriptions. Additionally, MTMs provide Targeted Medication Reviews (TMRs) to continuously identify and resolve medication-related problems. MTMs are critical for developing customized interventions to help members overcome barriers to adherence, identify gaps in therapy and screen for medication safety concerns while coordinating care with prescribers.
Academic detailing
Cost can be a barrier to adherence. However, PBMs have unique insights into near real-time claims data to identify prescribing patterns that put members at risk for low medication adherence. Academic detailing involves analyzing this data to recognize members on high-cost medications that could be switched to equally effective, lower-cost formulary alternatives. Making the drug more affordable, can help members stay adherent. At Navitus, in addition to our pharmacy and therapeutics (P&T) committee, our drug information department continuously reviews and revises plan sponsors’ drug formularies, as needed, to replace higher-cost medications with lower-cost options. Then, trained health care professionals educate prescribers on clinically effective, less expensive alternatives to change prescribing patterns, resulting in reduced costs for both the plan sponsor and member. This individual outreach also improves care by promoting prescribing that is consistent with medical evidence.
personalized member transitions
Plan or formulary changes that occur when a plan sponsor starts working with a new PBM partner can be confusing for members and result in gaps in care or member disruption, creating opportunities for non-adherence to creep in. A PBM with a high-touch, personalized onboarding and transition experience for members and plan sponsors can ease concerns during the switch. To ensure a smooth process for all entities involved, plan sponsors should consider what programs and strategies their PBM partner has to create a positive and seamless benefits transition experience. For example, Navitus’ Clinical Engagement Center prevents gaps in therapy for members with chronic conditions by improving speed to fill prescriptions and helps members navigate the health care system with personalized pharmacist-led support and proactive multi-channel communications.
Medication non-adherence is a widespread issue. With the right PBM partner, plan sponsors can successfully navigate these challenges with Medication Therapy Management, Academic Detailing and Personalized Transition Services to prevent poor health outcomes, reduce medication non-adherence and achieve lower plan costs.
|
|
Written by Julie Olson, DNP, MS, RN, CQIAJulie is Navitus' Senior Director of Population Health where she leads a team of pharmacists and product managers to design, implement and execute clinical programs on behalf of Navitus and Lumicera Health Services. She has nearly 30 years of diverse health care experience, including public health nursing, health outcomes research, public policy analysis, and business development. |





